At Oncode Institute, we focus on turning cancer research into real-world results for patients. Our programmes accelerate the journey from discovery to better treatments, helping to improve cancer care, reduce side effects, and increase access for everyone affected by cancer.
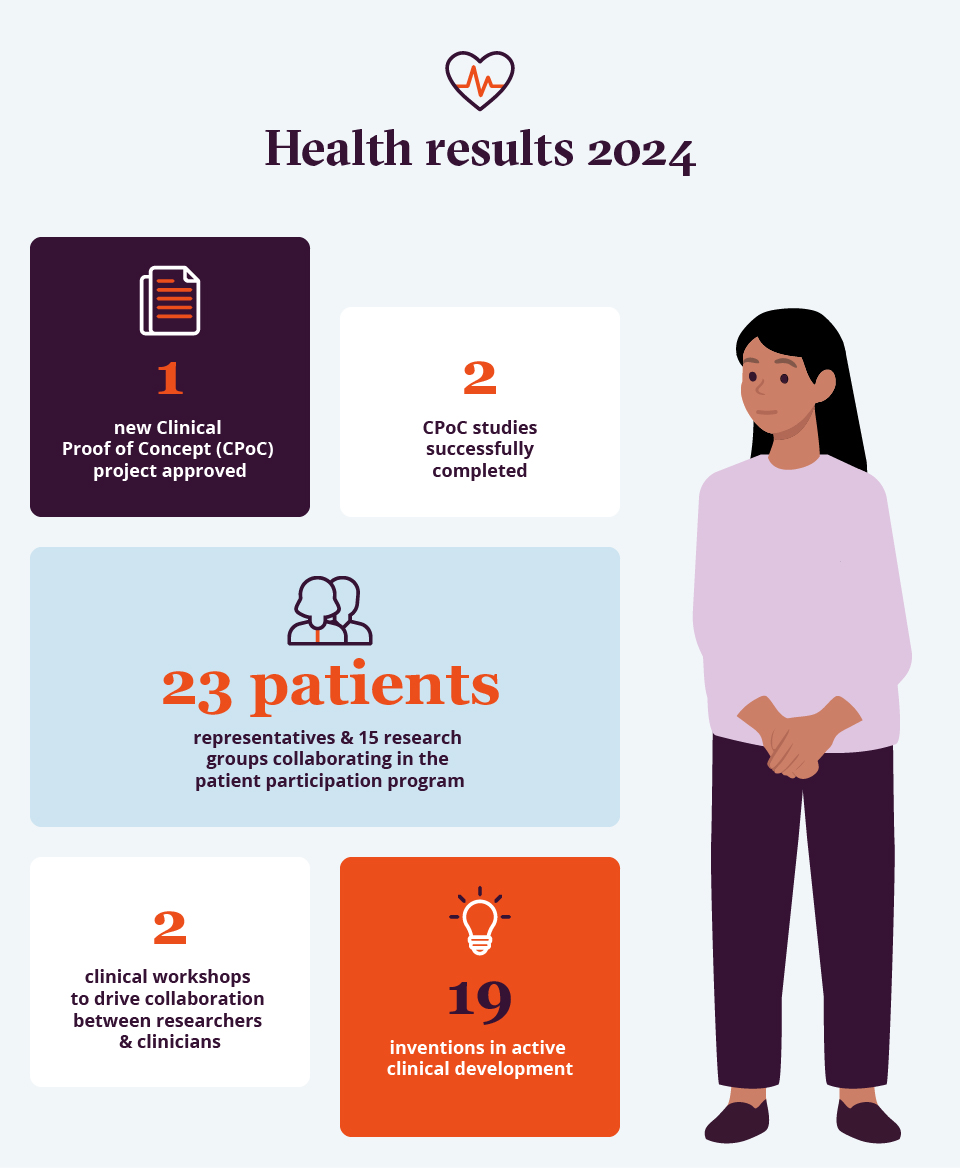
With support from our Clinical Proof-of-Concept Fund, researchers can test promising discoveries in early clinical trials. This bridges the gap between laboratory findings and patient benefit. Our Base Research Funding gives scientists the freedom to explore bold ideas and the flexibility to act on them.
Together, these resources help turn innovation into action. Our valorisation support ensures that promising diagnostics and therapies do not remain on the shelf, but reach the clinic where they can make a real difference.
We focus on precision: treatments that are more effective, with fewer side effects. We also support advanced approaches to diagnose cancer earlier, and match patients with the right therapy.
Every day counts - for patients, families and the future of cancer care.
A Healthier Future
Our impact goes beyond developing better treatments. We are equally committed to making healthcare more accessible and sustainable.
This means accelerating treatment optimisation, reducing unnecessary costs and exploring new uses for existing drugs through drug repurposing. These approaches save valuable time and resources while offering new hope to patients.
Impact Story
Patient Perspective.
Patients and researchers work together in Oncode Institute’s Patient Perspective Programme. For example, patients Carolien Hovenier and Theo Theunissen collaborate with Oncode Institute researchers Michiel Vermeulen, Suzanne Weijers and Geert Litjens.
Carolien Hovenier became involved in Michiel Vermeulen’s research group in 2023 to learn more about preclinical research. ‘I increasingly realised that effective treatments originate in the lab,’ she says. ‘Not only the development of new drugs, but also improvements to medicines currently prescribed. I wanted to contribute to linking preclinical research to clinical research and vice versa.’
Hovenier participates because she believes patients should experience fewer side effects. ‘Now and then, my bone marrow has a hard time. This reduces my immune system, so I must always keep my distance and avoid crowded places. I also experience a lot of stress before visits to the oncologist. This has a considerable impact on my life,’ she explains.
Suzanne Weijers - a researcher in the Vermeulen lab - values this patient input: ‘Thanks to Carolien’s story, I gained more insight into the impact of side effects and what I can do to minimise them.’
‘Being ill and getting better do not come for free,’ says patient Theo Theunissen. After a stroke led to the discovery of a neuroendocrine tumour, he was inspired to develop a system to help people improve walking at home following a stroke. He contacted Oncode Investigator Geert Litjens. ‘Theo spoke to our PhD students about his cancer and, drawing on his professional expertise, contributed ideas about the practical application of our AI models,’ says Litjens. ‘Thanks to his contribution, passion and personal experiences, we can focus on developing methods that make a difference for patients with prostate cancer.’
By facilitating direct collaboration between patients and scientists, Oncode Institute strengthens the connection between research and clinical practice. Vermeulen emphasises: ‘Talking to patients gives our research a face. Their personal experiences and critical questions take scientific research to a higher level.’
We also invest in technologies that improve patient stratification - grouping patients by genetic markers, disease subtype or other characteristics - ensuring each patient receives a treatment plan tailored to their specific condition. One such innovation is Sturgeon, a tool that enables brain surgeons to operate with greater precision. Just two years after its development, Sturgeon is already being used to treat children with brain tumours, and is now being adapted for adult care.
Through collaborations with hospitals, biotech companies and academic partners, we continue to scale our efforts and expand our reach. These strategic partnerships allow us to deliver solutions to more patients - faster and more effectively.
At Oncode Institute, we are not only working to cure cancer: we are building a future where cancer care is smarter, fairer and accessible to everyone.
Oncode Institute: outsmarting cancer, impacting lives


Voices From Our Community
Rebekka Schneider, Oncode Institute Investigator:
‘Bringing our research results to the clinic has always been my dream. With the launch of the TasquForceMPN study* in collaboration with HOVON, that dream has become a reality. Thanks to the support of Oncode Institute, we can now use our extensive single-cell RNA data from patients in innovative ways - accelerating the translation of research into clinical practice.’
* TasquForceMPN study: a clinical trial testing a new drug - tasquinimod - in patients with myelofibrosis who have not responded to standard treatment. It aims to improve symptoms, reduce spleen size and explore new ways to target the disease.
Joachim Aerts, Professor of Pulmonary Medicine, Erasmus MC:
‘There is great interest in research among doctors, but most lack the time and resources to pursue it. As a result, many brilliant ideas never make it past the pipeline. For a project like the TEIPP Trial*, you need someone who recognises the value of clinical research, dares to translate it into practice, and takes responsibility for driving the trial forward. This is where the Clinical Proof-of-Concept programme truly makes the difference. When an unexpected clinical response occurs, you must act fast to maintain momentum. Thanks to Oncode Institute, we were able to do exactly that. The role of doctors who can translate research findings into successful trials is often underestimated. That is why our partnership with Oncode Institute is so powerful.’
*TEIPP Trial: a clinical study testing new ways to treat cancer by turning lab discoveries into real treatments for patients. It brings together researchers, clinicians and patients to ensure findings are applied effectively in care.
Eelco Hoving, Paediatric Neurosurgeon and Clinical Director of Neuro-oncology at the Prinses Máxima Center:
‘During surgery, we sometimes deliberately leave a small amount of tumour tissue behind to prevent damage to the brain. However, if it later proves to be an aggressive tumour, a second operation may be necessary, bringing additional risks and a great deal of stress for the child and their family. Thanks to rapid DNA analysis, we can now identify the type of tumour during the first operation. Sturgeon technology allows us to make safer, more precise decisions at the right time.’